Save Yourself From These Three Harmful Effects Of Poor Sleep
Sleep is a state of unconsciousness where an individual can be woken at any moment as their brain and body are still active. It can also be viewed as the period in which various restorative processes like wound healing, homeostatic balance, and other metabolic processes occur. However, in recent years, people have been complaining of sleep deprivation or chronic sleep loss. This happens mostly due to our sedentary lifestyle and other factors such as depression, schizophrenia, cancer, stroke, chronic pain syndrome, and Alzheimer's disease.
- Sleep Loss And Its Consequences
- Cortisol And Insomnia
- Poor Sleep And Insulin-Resistance
- Poor Sleep Leads To Weaker Bones, Muscles And Aged Skin

Sleep deprivation (or insomnia; in chronic conditions) happens when the quantity, as well as the quality of sleep are compromised. The unfavourable effects of sleep loss on the immune and endocrine systems are sparsely available but it is important to evaluate and understand the behaviour and consequences of less sleep.
Sleep Loss And Its Consequences
The immune system protects the internal biological environment by preventing foreign invasions. Adequate sleep promises that the immune system and its products are efficiently working and being produced to ward off diseases. Sleep period helps in the recovery of health and restores homeostatic conditions, so variability in the sleep duration does impact our immunological pathways.
Along with the immune system, the endocrine system also manages homeostasis and the internal environment. The wake and sleep times are important in the release of hormones, and vice-versa. Melatonin, cortisol, and sex hormones like progesterone and oestrogen are said to be vital to the sleep-wake cycle.
Let us learn more about poor sleep.
Cortisol And Insomnia
Cortisol is the stress hormone that affects the sleep cycle and the body’s circadian rhythms, along with melatonin. The levels of this hormone rise and fall so that an individual can have a proper sleep schedule and sound sleep. This is because cortisol triggers the fight-or-flight response and prevents sleep inertia, therefore, it is highest in the morning. It has a 24-hour cycle or circadian rhythm wherein it peaks during the early morning hours and gradually declines throughout the day, being the lowest at night.
Due to poor sleep or insomnia, elevated cortisol levels will prevail in the body and thus, a person will find it difficult to sleep at night. Suppose, a person has 20 units of cortisol in the morning; it drops to two units by the night—this may allow a person to sleep peacefully. Studies have shown that if a person is deprived of 4-5 hours of sleep for a single night, the cortisol levels will rise by approximately 20–30% the next day. These levels will then disrupt the sleep cycle, leading to a vicious cycle of disrupted sleep schedules.
Sleep-deprived individuals or patients suffering from insomnia are observed to have high cortisol levels in the evening or before bedtime. Thus, it can be said that cortisol, or the stress hormone, influences the sleep cycle and is one of the causes of insomnia. It increases the sleep debt and decreases the next-day energy levels. To combat the energy, cortisol level rises and this is explained in detail in the next section.
Also, Read | How Do Hormones Affect Your Weight?
Poor Sleep And Insulin-Resistance
A poor sleep cycle can make you insulin resistant. Yes, that’s right! Cortisol level rises in the morning or just before we wake up as it adds sugar to the blood. This is required to provide energy to the body, and thus the hormone is also known as glucocorticoid. Poor sleep will disturb the circadian rhythm, which will eventually affect cortisol levels. Due to less sleep, cortisol levels will rise to keep the body alert, and it will also add more sugar in the bloodstream to keep up with the energy levels. As a result of this, the effects of insulin will be compromised, leading to low insulin sensitivity or insulin resistance.
Insulin is the hormone that pulls out sugar from the bloodstream or processes the blood sugar. In a sleep-deprived person, there will be a glucocorticoid overload that counteracts the insulin effects so that more sugar is present for energy and alertness. Hence, poor sleep naturally causes insulin resistance, due to which an individual will produce more insulin than is required to process the food taken throughout the day.
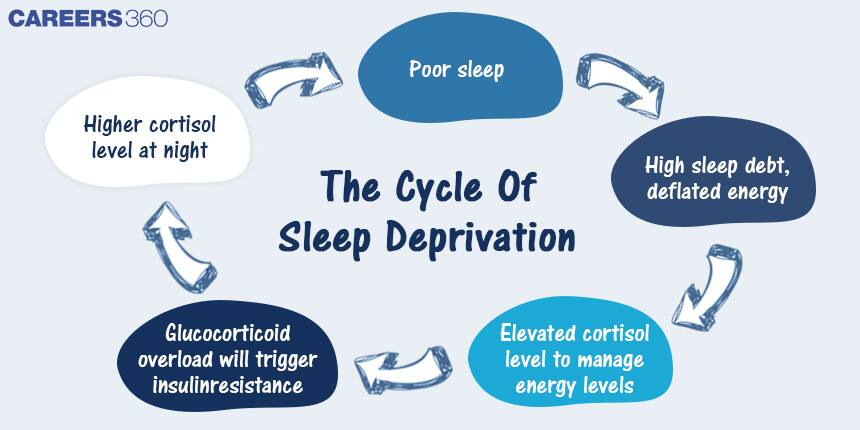
Poor sleep and cortisol relationship is depicted above
Poor Sleep Leads To Weaker Bones, Muscles And Aged Skin
Cortisol is a catabolic hormone, which means it triggers the breakdown of molecules. As the hormone levels are chronically high in poor sleep, we tend to break down more molecules to sustain. But what exactly is being broken down?
During catabolic or high cortisol levels, the body tends to decompose proteins to obtain more amino acids (protein’s basic unit) in order to convert them into fuel. Collagen and muscle proteins are a few examples that are broken down to produce amino acids.
Collagen is the growing tissue that forms a soft framework in bones and is a fundamental part of the skin. During high cortisol levels, or the catabolic phase, the collagen protein is broken down into peptides, and subsequently, people will have wrinkled skin. Similarly, muscle protein is also used to produce amino acids for fuel. Undoubtedly, this will lead to weaker muscles and a thinner body. The bones will be brittle due to the tearing down of bones in the catabolic phase.
Chronic cortisol elevation due to poor sleep can be termed a destructive survival mechanism, as it produces not one but multiple disorders in the body. Sleep loss outcomes range from mild to adverse, like the common cold, postpartum depression, insulin resistance, obesity, organ damage, degeneration of brain functions, and many more.
Therefore, the biological consequences of sleep loss should be comprehensively considered. Some variables of poor sleep cannot be modified; many factors, however, can be changed. It is of utmost importance that the sleep schedule be fixed and followed so as to fix the biological clock. The immediate and long-term effects of sleep deprivation can be avoided by successfully focusing on the quantity and quality of sleep. One must consider sleep continuity, sleep environment, sleep duration, sleep disruptors, and other related factors to deal with poor sleep.
Also, Read | Insulin Sensitivity And Its Effect On Hormones
Articles
Upcoming Exams
Application Date:20 January,2025 - 18 April,2025